Scientific evidence on medication adherence confirms that Artificial Intelligence significantly improves patient compliance through personalized, data-driven interventions. AI-powered tools use predictive analytics and real-time feedback from smart devices to offer proactive support, proving more effective than traditional methods and leading to better health outcomes.
Advertisement
In today’s digital age, medication adherence research shows AI can transform patient care. Have you ever wondered how scientific evidence shapes health outcomes? Keep reading to explore these insights.
introduction to ai in medication adherence
Medication adherence, or how well patients follow their prescribed treatment plans, is a major challenge in healthcare. When people don’t take their medications as directed, it can lead to poor health outcomes and higher medical costs. Traditional methods like simple reminders or pillboxes have limitations and often don’t address the root causes of non-adherence.
This is where Artificial Intelligence (AI) comes in. AI offers a smarter, more personalized way to support patients. Instead of one-size-fits-all reminders, AI systems can learn an individual’s habits and routines to provide timely and effective support. Using machine learning algorithms, AI can predict who is at risk of missing a dose and intervene before it happens.
How AI Transforms Adherence
AI-powered tools go beyond basic alarms. They can include smart pill dispensers that release medication at the right time, mobile apps that send interactive reminders, and even virtual assistants that answer questions about treatment. These systems can track adherence data in real-time, providing valuable insights for both patients and healthcare providers. This allows for quick adjustments to care plans, making treatment more effective and personalized.
By analyzing patterns in behavior, AI helps uncover the specific barriers each person faces. For example, it might identify that a patient often forgets their evening dose due to a busy schedule. In response, the AI could suggest a different time or send a reminder that aligns with their daily activities. This level of customization is key to improving long-term medication adherence and overall health.
Advertisement
overview of scientific evidence
A growing body of scientific research confirms that Artificial Intelligence can significantly improve medication adherence. Studies published in various medical journals are providing solid evidence that AI-driven interventions are more effective than traditional methods. These studies often compare groups using AI tools against control groups using standard reminders or no intervention at all.
The findings consistently show that personalized, adaptive support powered by AI leads to better outcomes. Patients using these advanced systems are more likely to take their medications correctly and on time. Evidence from randomized controlled trials highlights that AI platforms can increase adherence rates by a notable margin, making a real-world impact on patient health.
Key Research Findings
Clinical studies often measure success using metrics like the Medication Possession Ratio (MPR), which tracks how often a patient has their medication available. Research shows that AI-powered apps and devices lead to higher MPR scores. Furthermore, the evidence points to the power of predictive analytics. AI can identify patients at high risk of non-adherence, allowing healthcare providers to intervene proactively before a problem occurs. This targeted approach is far more efficient than broad, non-specific reminders.
The Strength of Data-Driven Insights
Scientific evidence also supports the value of the data collected by AI systems. This information provides healthcare professionals with a clear view of a patient’s adherence patterns over time. Instead of relying on patient memory or self-reporting, which can be inaccurate, doctors can see objective data. This allows for more informed conversations and adjustments to treatment plans, creating a collaborative and effective approach to care.
role of ai in healthcare
Artificial Intelligence is changing the entire landscape of healthcare, far beyond just helping patients remember their pills. It’s becoming a vital tool for doctors, researchers, and hospitals. From diagnosing diseases earlier to discovering new drugs, AI is driving innovation across the board. For instance, AI algorithms can analyze medical images like X-rays and MRIs with incredible accuracy, often spotting issues that the human eye might miss.
This technology also plays a crucial role in creating personalized treatment plans. By analyzing a patient’s genetic information, lifestyle, and medical history, AI can help doctors recommend the most effective therapies for that individual. This moves healthcare away from a one-size-fits-all approach to something far more precise and effective.
From Diagnosis to Daily Management
One of AI’s greatest strengths in healthcare is its ability to process massive amounts of data in seconds. A doctor can’t possibly read every new medical study, but an AI can. This provides clinicians with powerful decision support tools, offering up-to-date insights and recommendations right when they need them. This support helps improve diagnostic accuracy and optimize treatment strategies.
The same technology that powers these complex tasks is also used to support daily patient management, including medication adherence. Think of it as part of a connected ecosystem. The AI that helps create a treatment plan can also help ensure the patient follows it. By enabling continuous remote monitoring through wearable devices and apps, AI keeps healthcare providers informed about a patient’s progress and can alert them to potential issues, making proactive care the new standard.
understanding medication adherence
Medication adherence simply means taking your medications exactly as prescribed by your doctor. This includes taking the right dose, at the right time, and in the right way. It might sound simple, but it’s one of the biggest challenges in healthcare. Failing to adhere to a medication plan, known as non-adherence, can lead to serious health problems, disease progression, and even hospitalization.
Non-adherence is not just about being forgetful. It’s often a complex behavioral issue influenced by many factors. For many people, juggling multiple medications with different schedules can be confusing and overwhelming. This is especially true for those with chronic conditions who need long-term treatment.
Common Barriers to Adherence
Several obstacles can prevent someone from following their medication plan perfectly. These can include:
- Forgetfulness: A simple memory lapse is the most common reason.
- Complex Regimens: Having to take many different pills at various times of the day.
- Side Effects: Unpleasant side effects can make people want to stop their medication.
- Cost: High prescription costs can be a significant barrier for many.
- Lack of Understanding: Not fully grasping why the medication is necessary or how it works.
Understanding these barriers is the first step toward finding effective solutions. The success of any medical treatment doesn’t just depend on the drug itself; it directly impacts treatment success and relies heavily on the patient’s ability to follow the plan consistently.
methods for data collection in research
To measure if AI truly helps with medication adherence, researchers need accurate and reliable data. Traditional methods, like asking patients to report their own behavior (self-reporting) or manually counting leftover pills, have major drawbacks. They can be inaccurate because people forget, or they may not want to admit they missed a dose.
Modern research, especially studies involving AI, relies on more advanced and objective data collection methods. These digital tools provide a continuous stream of information without relying on a patient’s memory. This shift to objective data is crucial for generating high-quality scientific evidence.
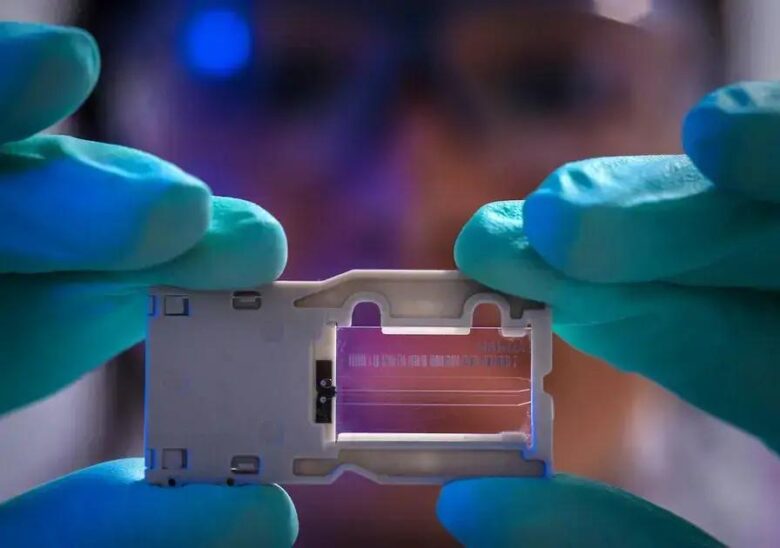
Modern Data Collection Techniques
Researchers now use a variety of technologies to track adherence in real-time. These include:
- Smart Pill Bottles: These devices have caps that record the exact time and date they are opened, creating a reliable log of when medication was accessed.
- Mobile Health Apps: Patients can use apps to log when they take their medication. The apps can also send reminders and gather feedback, providing rich, interactive data.
- Wearable Sensors: Some technologies involve patches or other wearables that can detect when a medication has been taken, offering direct biological confirmation.
- Digital Pharmacy Records: AI can analyze pharmacy refill data to identify when patients are late to pick up their prescriptions, which is a strong indicator of non-adherence.
By combining data from these different sources, AI can build a comprehensive and highly accurate picture of a patient’s adherence behavior, which is essential for effective research and analysis.
analyzing adherence rates via ai
Once the data is collected, the real power of Artificial Intelligence comes into play. AI doesn’t just count missed doses; it dives deep into the data to understand the ‘why’ behind a patient’s behavior. Using advanced machine learning algorithms, AI can process vast and complex datasets from multiple sources—like smart pill bottles, apps, and pharmacy records—all at once. This allows it to see connections and patterns that would be impossible for a human to spot.
The goal is to turn raw data into meaningful information. For example, the AI might notice that a patient consistently forgets their medication on weekends or right before a prescription refill is due. This level of detailed analysis helps build a personalized understanding of each patient’s challenges.
From Patterns to Predictions
The most significant part of analyzing data with AI is its predictive capability. Instead of just reacting to non-adherence after it happens, AI can forecast it. By learning from the behavior patterns of thousands of patients, it can create predictive models that identify individuals at high risk of missing their medication in the future. This allows healthcare providers to be proactive.
For instance, an AI system might flag a patient whose app usage has recently dropped, suggesting they may be losing motivation. This triggers an alert for a healthcare provider to check in, offering support before adherence becomes a major issue. This proactive approach, driven by intelligent analysis, is what makes AI a game-changer for improving health outcomes.
comparison of traditional vs ai methods
Traditional methods for encouraging medication adherence have been around for decades. These include simple tools like weekly pill organizers, calendar reminders, or basic alarms on a clock or phone. While better than nothing, these methods share a common flaw: they are static and passive. They rely entirely on the patient’s own motivation and memory to be effective. They offer a one-size-fits-all solution that doesn’t adapt to an individual’s unique needs or lifestyle.
Furthermore, traditional methods provide no feedback loop. A doctor has no way of knowing if a patient is using their pillbox correctly or ignoring their alarms. This lack of data makes it impossible to intervene until the patient’s health has already been affected.
The AI Advantage: A Dynamic and Proactive Approach
AI methods, in contrast, are dynamic and proactive. Instead of a simple, fixed alarm, an AI-powered app can learn when a patient is most likely to forget and send a personalized reminder at just the right moment. AI systems create a continuous feedback loop, collecting real-time data on adherence that can be shared with healthcare providers. This allows for timely conversations and adjustments to care.
While a pillbox simply holds pills, a smart dispenser can track when it’s opened and even notify a caregiver if a dose is missed. The core difference is intelligence: traditional methods are tools, whereas AI methods are partners in a patient’s health journey, offering personalized support and predictive insights that were previously impossible.
impact of ai on patient outcomes
When patients use AI to improve their medication adherence, the impact on their health is direct and powerful. Better adherence leads to better management of chronic conditions like diabetes and high blood pressure. This means fewer health complications, a lower risk of disease progression, and a significant reduction in emergency room visits and hospital stays. The ultimate goal of any health intervention is a better quality of life, and AI is proving to be a key tool in achieving that.
The impact goes beyond just taking pills correctly. The data gathered by AI systems gives healthcare providers a clear window into a patient’s daily routine. This allows them to step in with support before a small issue becomes a big problem. For example, if a patient’s adherence starts to slip, a nurse can be notified to reach out. This proactive approach prevents health setbacks and keeps patients on track.
Tangible Benefits for Patients
The use of AI to support medication adherence translates into real-world improvements in patient health. Key outcomes include:
- Better Chronic Disease Control: Stable blood sugar levels for diabetics or controlled blood pressure for hypertensive patients.
- Reduced Hospital Readmissions: Patients who follow their post-discharge medication plans are less likely to be readmitted.
- Increased Patient Empowerment: By being more involved in their treatment, patients feel more in control of their health.
- Enhanced Safety: AI can help manage complex medication schedules, reducing the risk of accidental double-dosing or missed doses.
case studies and success stories
The scientific evidence is brought to life through real-world examples of how AI is helping patients every day. These success stories show the practical impact of using intelligent technology to manage medication adherence, moving from theory to tangible results.
Case Study: Better Diabetes Management
Consider a patient with type 2 diabetes who struggled to manage multiple daily medications and insulin injections. By using an AI-powered mobile app, they received personalized reminders that adapted to their daily schedule. The app also allowed them to log their blood sugar readings alongside their medication intake. The AI analyzed this data, revealing a pattern between late evening doses and high morning blood sugar levels. This insight, shared with their doctor, led to a simple adjustment in their treatment plan. As a result, the patient achieved better glycemic control and felt more empowered in managing their condition.
Success Story: Preventing Hospital Readmission
Another powerful example involves an elderly patient recovering from heart surgery. They were discharged with a complex regimen of critical medications. A smart pill dispenser, connected to a telehealth platform, was provided. One afternoon, the AI system detected that a crucial anti-clotting medication had not been taken. It automatically sent an alert to the patient’s phone and, after no response, notified a remote monitoring nurse. The nurse called the patient, who had simply fallen asleep and forgotten. This immediate, proactive intervention helped prevent a potentially life-threatening complication and avoided a costly hospital readmission.
challenges in ai implementation

While the benefits of AI are clear, integrating it into the complex world of healthcare presents real challenges. Successfully implementing these technologies requires careful planning to overcome several technical, practical, and human-centered hurdles. These obstacles must be addressed for AI tools to be truly effective and widely adopted.
Key Implementation Hurdles
Navigating these obstacles is a critical step for any healthcare organization. The primary challenges include:
- Data Privacy and Security: Patient health information is highly sensitive. Any AI system must use robust security measures and comply with strict regulations like HIPAA to protect sensitive health data from breaches.
- Integration with Existing Systems: Hospitals rely on complex Electronic Health Record (EHR) systems. Making a new AI platform work seamlessly with these legacy systems is often difficult and expensive, yet seamless integration is crucial for a unified view of patient care.
- User Adoption and Trust: Technology is only effective if people are willing to use it. Some patients, particularly older adults, may be hesitant to adopt new apps or devices. Likewise, clinicians need to be trained to trust and effectively use the insights provided by AI.
- Cost and Scalability: The initial investment for developing and deploying a sophisticated AI adherence program can be high. Ensuring the solution is not only affordable but also scalable to serve a large patient population is a significant consideration.
regulatory considerations and compliance
When using Artificial Intelligence in healthcare, it’s not enough for the technology to be smart; it must also be safe and legal. All AI tools that handle patient information must operate within a strict framework of rules and regulations. This is essential to protect patient privacy and ensure the technology is used responsibly.
The most important regulation in the United States is the Health Insurance Portability and Accountability Act, better known as HIPAA. This law sets the standard for protecting sensitive patient health information. Any app, device, or platform using AI for medication adherence must be fully HIPAA-compliant.
Navigating the Regulatory Landscape
Beyond HIPAA, there are other key considerations that developers and healthcare providers must address:
- FDA Oversight: If an AI tool does more than just remind—for instance, if it analyzes data to provide medical advice—it may be classified as a medical device. In such cases, it could require clearance or approval from the Food and Drug Administration (FDA) to ensure it is safe and effective.
- Data Consent and Transparency: Patients have a right to know how their data is being collected, used, and protected. Gaining clear consent is not just a legal requirement; it’s fundamental to building trust between the patient and the technology.
- Algorithm Fairness: The AI must be designed and tested to ensure it works equally well for all patient populations, without introducing any bias based on race, age, or socioeconomic status.
Ensuring compliance from the very beginning of development is critical. Building technology with a ‘privacy-by-design’ approach is the only way to earn the trust of both patients and regulators.
advancements in ai technology for healthcare
Artificial Intelligence in healthcare is not standing still; it’s evolving at an incredible pace. The technology used to support medication adherence today is far more advanced than the simple reminder apps of a few years ago. Current advancements are focused on making AI smarter, more conversational, and deeply integrated into a patient’s overall health picture.
Instead of just sending notifications, modern AI systems are becoming true health companions. They use more sophisticated machine learning models to understand not just *if* a patient took their medicine, but the context surrounding their actions. The goal is to move from simple tracking to genuine understanding and support.
Smarter, Conversational AI
One of the biggest advancements is in Natural Language Processing (NLP). This allows AI-powered chatbots and virtual assistants to have more human-like conversations. A patient can ask questions like, “Is it okay to take this pill with food?” and get an intelligent, helpful response. This creates a more engaging and supportive experience than a simple alarm ever could.
From Predictive to Prescriptive
Early AI could predict who was at risk of non-adherence. The next generation of AI is moving toward prescriptive analytics. This means it doesn’t just flag a problem; it suggests the best possible solution for that specific individual. For example, based on a patient’s habits, it might recommend changing a dose time or offer educational content to address their specific concerns. This level of personalization is a major leap forward.
the importance of research confirmation
A new technology might seem promising, but in healthcare, promises are not enough. Every claim, especially for a tool as powerful as AI, must be proven with solid, scientific evidence. Research confirmation is the process of rigorously testing an AI solution to verify that it actually works as intended and is safe for patients. This is what separates a trendy gadget from a trustworthy medical tool.
Without this validation, we are just guessing. Scientific confirmation through clinical trials and peer-reviewed studies provides the necessary proof that an AI tool can reliably improve medication adherence. It builds the foundation of trust for everyone involved.
The Gold Standard for Trust and Adoption
Research confirmation is essential for several key reasons:
- For Clinicians: Doctors and nurses rely on evidence-based medicine. They need to know that the tools they recommend to patients are backed by credible data showing they improve health outcomes.
- For Patients: Knowing that an app or device has been scientifically validated gives patients the confidence to trust it with their health.
- For Healthcare Systems: Hospitals and insurance providers require proof of effectiveness before they will invest in and adopt new technologies on a large scale. Reproducible positive results are necessary to justify the cost and effort of implementation.
Ultimately, research confirmation ensures that the focus remains on what truly matters: improving patient health in a way that is safe, effective, and reliable.
implications for healthcare providers
The rise of AI in medication adherence doesn’t replace healthcare providers; it equips them with powerful new tools. For doctors, nurses, and pharmacists, this technology transforms their role from being reactive to proactive. Instead of only finding out about non-adherence when a patient’s condition worsens, they can now see real-time data and intervene early.
This shift allows providers to manage their patient populations more effectively. AI acts as a digital assistant, monitoring adherence in the background and flagging only those patients who need immediate attention. This frees up valuable time for providers to focus on more complex clinical tasks and meaningful patient interactions.
A Shift to Proactive and Personalized Care
AI-driven tools have several direct implications for the daily work of healthcare professionals:
- More Meaningful Consultations: Providers can have more informed conversations with patients, using objective data about adherence patterns rather than relying on memory or self-reporting. This leads to more effective, targeted advice.
- Efficient Workflow: By identifying high-risk patients, AI helps providers focus their efforts where they are most needed. This is especially valuable in busy clinical settings, improving efficiency without sacrificing quality of care.
- Improved Care Coordination: When the entire care team—from the primary care doctor to the pharmacist—has access to the same adherence data, they can work together more seamlessly to support the patient.
future trends in ai-driven adherence
The evolution of AI in medication adherence is pointing towards a future where support is not just smart, but almost invisible and perfectly woven into our daily lives. The trend is moving away from standalone apps and devices toward a fully integrated health ecosystem. Future AI will know more about a patient’s context, making support more timely and effective than ever before.
Imagine an AI that doesn’t just remind you to take a pill, but knows you have an early meeting and adjusts its timing accordingly. The goal is to create a truly personalized and proactive health partner that anticipates needs before they arise.
What’s on the Horizon?
Several exciting trends are shaping the future of AI-driven adherence:
- Hyper-Personalization: AI will connect to more data sources like calendars, fitness trackers, and even sleep monitors to deliver hyper-personalized support that fits seamlessly into a person’s unique lifestyle.
- Voice and Conversational AI: Interacting with adherence support will become as easy as talking. Patients will be able to ask smart speakers like Alexa or Google Assistant, “Did I take my morning pills?” and get an intelligent response.
- Advanced Behavioral Science: AI will incorporate more sophisticated behavioral science principles, using gamification, rewards, and positive reinforcement to motivate patients in a way that is tailored to their personality.
- Deeper Wearable Integration: Future AI will use data from wearables not just for reminders, but to correlate adherence with real-time biometric data like heart rate or blood pressure, providing a complete picture of treatment effectiveness.
ethical considerations in ai usage
Using AI in healthcare brings up important ethical questions that go beyond technology. As we rely on these smart systems to help with personal health, we must ensure they are used in a way that is fair, safe, and respectful to every individual. This means carefully thinking about the moral implications of how patient data is handled and how AI influences decisions.
The core of the issue is trust. Patients will only embrace these tools if they are confident that the technology is working in their best interest and respecting their rights. Building this trust requires a commitment to ethical principles from the very start.
Key Ethical Considerations
Several critical ethical questions must be addressed:
- Data Privacy and Consent: Who owns the vast amount of personal health data collected by AI? Patients must have clear, transparent control over their information, understanding exactly how it will be used and shared.
- Algorithmic Bias: AI learns from data. If the data it’s trained on primarily represents one group of people, the AI might not work as well for others. This could accidentally worsen health disparities for minority groups, the elderly, or those with lower incomes.
- Accountability: If an AI system makes a mistake—like providing incorrect information or failing to send a critical alert—who is responsible? The developer, the doctor who recommended it, or the hospital? Defining accountability is a major ethical hurdle.
- Patient Autonomy: There’s a fine line between a helpful nudge and a manipulative push. AI should empower patients with information and support, not pressure them or take away their right to make their own choices. Respecting a patient’s autonomy is paramount.
best practices for implementing ai
Implementing AI in healthcare requires a careful, strategic approach to ensure it’s both effective and trusted. Simply introducing a new technology is not enough; success depends on a thoughtful plan that puts users at the center. Following best practices is key to bridging the gap between a promising AI tool and real-world improvements in medication adherence.
Key Steps for Successful Implementation
To ensure a smooth and effective rollout, healthcare organizations should follow a clear roadmap:
- Start with a Specific, Measurable Goal: Begin with a well-defined objective. For example, focus on improving adherence for a high-risk patient group, like those with newly diagnosed diabetes, rather than trying to solve everything at once.
- Prioritize Patient-Centered Design: The technology must be incredibly easy to use for everyone, including patients who are not tech-savvy. A user-friendly interface is essential for adoption and long-term engagement.
- Ensure Seamless Integration: The AI tool must connect smoothly with existing clinical workflows and Electronic Health Records (EHRs). This prevents creating extra work for providers and ensures data is accessible where it’s needed most.
- Provide Robust Training and Support: Both clinicians and patients require thorough training. Doctors and nurses need to trust the AI’s insights, and patients need to feel confident using the technology. Ongoing support is crucial.
- Run a Pilot Program First: Before a large-scale launch, test the solution with a smaller group. This allows the team to gather feedback, work out any bugs, and prove the tool’s value in a controlled environment.
emerging insights and ongoing research
The field of AI in medication adherence is constantly evolving, with researchers continually uncovering new insights. Current studies are moving beyond simply tracking if a dose was taken. They are now exploring the deeper ‘why’ behind patient behaviors and how to create even more intelligent and predictive support systems.
Ongoing research is focused on building a more holistic view of the patient. This involves integrating diverse types of data to understand the complex factors that influence adherence. The goal is to not just remind, but to truly understand and anticipate a patient’s needs.
New Frontiers in Adherence Research
Scientists are actively exploring several cutting-edge areas:
- Behavioral Phenotyping: Researchers are using AI to identify distinct behavioral patterns or ‘phenotypes’ among patients. This allows for the creation of targeted interventions designed for specific types of non-adherence, such as ‘forgetful but willing’ versus ‘intentionally skipping due to side effects’.
- Pharmacogenomic Integration: A groundbreaking area of research involves combining adherence data with a patient’s genetic information. This could help predict not only who will struggle with adherence but also who is more likely to experience side effects, allowing for proactive medication adjustments.
- The Rise of Digital Twins: Perhaps one of the most futuristic concepts being researched is the creation of ‘digital twins.’ This involves building a dynamic, virtual model of a patient using their health data. Researchers can then simulate different adherence strategies on the digital twin to see what works best before applying it to the real person.
Harnessing AI for a Healthier Future
The scientific evidence is compelling and clear: Artificial Intelligence is a powerful and proven tool for improving medication adherence. It moves far beyond simple reminders, offering personalized, proactive support that adapts to the individual needs of each patient. This intelligent approach helps address the root causes of non-adherence in ways that traditional methods cannot.
As we’ve explored, the impact of AI leads to better patient outcomes, more efficient workflows for healthcare providers, and a more empowered role for patients in their own care. By turning real-time data into actionable insights, AI helps manage chronic conditions more effectively and can prevent serious health complications.
While challenges in implementation and ethics require careful consideration, the path forward is illuminated by ongoing research and technological advancements. The future promises even more integrated and intuitive solutions that fit seamlessly into our daily lives.
By embracing these scientifically validated tools, the healthcare community can take a significant step toward a future where every patient has the support they need to follow their treatment plans and achieve a better quality of life.
FAQ – AI and Medication Adherence
How does AI actually improve medication adherence?
Instead of simple alarms, AI uses personalized data to send smart reminders, predict when you might forget a dose, and provide real-time feedback to you and your doctor. It adapts to your specific routine and challenges.
Is there real scientific evidence that these AI tools work?
Yes, numerous clinical studies and research have shown that AI-driven interventions significantly increase medication adherence rates compared to traditional methods. This is confirmed using objective data from smart devices and apps.
Is my personal health data safe if I use an AI adherence app?
Reputable AI health tools are required to be compliant with strict privacy laws like HIPAA. They use strong encryption and security measures to protect your sensitive health information.
Will AI replace the role of my doctor or pharmacist?
No, AI is designed to be a tool that supports healthcare providers. It gives them better data to have more informed conversations with you, allowing them to provide more proactive and personalized care.
What are the biggest challenges to implementing AI in healthcare?
The main challenges include ensuring patient data privacy and security, integrating new AI systems with existing hospital records, overcoming user hesitation, and addressing potential biases in the AI algorithms.
What kind of future advancements can we expect in this area?
Future trends include hyper-personalization that connects to your daily calendar and fitness trackers, more advanced voice-controlled assistants, and deeper integration with wearable devices for a complete health picture.