Cumulative dosage caps are pre-set safety limits on the total amount of a medication taken over a specific period, used by healthcare systems and technology to prevent gradual drug accumulation in the body and flag potential overdose risks before they become dangerous.
Advertisement
When it comes to safe medication use, cumulative dosage caps offer a proactive approach. Have you ever wondered how small doses add up? This guide dives into practical methods to monitor and manage dosages.
understanding cumulative dosage caps
Understanding cumulative dosage caps begins with seeing medication intake over time, not just as single doses. A cumulative dose is the total amount of a specific drug a person takes over a set period, such as a week or a month. Think of it like a running total. Each pill or liquid dose you take adds to this total.
A ‘cap’ is simply a pre-determined safety limit on that total amount. It’s a ceiling that your total medication intake should not exceed within that timeframe to avoid potential harm. This is especially critical for medications that can build up in your system or have a narrow window between being effective and becoming toxic.
Why This Safety Net Matters
For many medications, a single dose is perfectly safe, but repeated doses can accumulate in the body. Over time, the concentration can reach dangerous levels, increasing the risk of an overdose or severe side effects. Cumulative dosage caps act as a crucial safety check, helping healthcare providers and patients monitor long-term treatment and prevent accidental overdose. They are a proactive tool for ensuring that a medication remains helpful without becoming harmful.
risks of overdose in medication management
The risk of an overdose isn’t always from a single, intentional act. More often, it’s an accidental overdose that occurs gradually through routine medication management. When multiple prescriptions are involved or when a single medication is taken for a long time, the potential for harm increases significantly if not carefully monitored. This risk isn’t limited to powerful painkillers; common medications can also accumulate to toxic levels in the body.
Factors That Increase Overdose Risk
Several factors can turn a safe prescription into a dangerous one. Mixing medications, a practice known as polypharmacy, can cause unpredictable interactions that intensify drug effects. A person’s health status also plays a huge role. For example, impaired kidney or liver function can slow down how the body processes a drug, causing it to build up over time.
Advertisement
Age is another critical factor. As we get older, our metabolism changes, which can affect how we respond to medication. What was once a safe dose may become risky. Without clear oversight and dosage caps, patients are left vulnerable to these hidden dangers, making proactive management essential for safety.
importance of dosage monitoring
Dosage monitoring is more than just taking pills on time; it’s a proactive safety measure that keeps a treatment plan effective and safe. By consistently tracking the amount of medication a person is taking, both patients and healthcare providers can spot potential issues before they become serious problems. This ongoing vigilance is the key to preventing accidental overdoses and ensuring the medicine is working as intended.
Key Benefits of Regular Monitoring
First and foremost, monitoring helps maintain a drug’s effectiveness. Many medications work best when they are kept at a stable level in the body, often called the therapeutic window. Too little, and the drug won’t work; too much, and it becomes toxic. Regular checks ensure you stay within this safe and effective range.
It also allows for personalized care. Every person metabolizes drugs differently based on age, weight, and overall health. What works for one person might be too much for another. Dosage monitoring provides the data needed to adjust prescriptions, tailoring the treatment directly to the individual’s needs and preventing cumulative harm.
evidence on cumulative effects
Scientific evidence clearly shows that the effects of many medications can build up over time. This isn’t just a theory; it’s a proven pharmacological principle. Long-term studies, known as longitudinal studies, track patients for months or even years. These studies consistently find that repeated exposure to certain drugs can lead to gradual changes in the body, sometimes resulting in unexpected side effects or toxicity that wasn’t apparent with short-term use.
From Lab Research to Patient Outcomes
The proof comes from multiple sources. In laboratory settings, researchers can observe how certain medications affect cells over extended periods. But the most powerful evidence comes from clinical data. For example, some heart medications, while effective, can slowly cause electrolyte imbalances if their cumulative dose isn’t monitored. Similarly, long-term use of certain painkillers can put a cumulative strain on the liver and kidneys.
This body of evidence is what informs the creation of cumulative dosage overdose caps. By analyzing data from thousands of patients, researchers can identify the threshold where a drug’s benefits are outweighed by its risks. This data-driven approach allows for the development of safety guidelines that protect patients from the hidden dangers of long-term medication use.
clinical practices and dosage caps

In daily clinical practice, dosage caps are not just abstract numbers; they are active safety tools integrated into healthcare systems. Modern electronic health records (EHRs) and pharmacy software often have built-in features that automatically track a patient’s medication history. These systems are designed to flag potential issues before they become dangerous.
How Clinical Decision Support Works
This automated safety net is known as clinical decision support. When a doctor prescribes a medication or a pharmacist goes to dispense it, the system cross-references the new prescription with the patient’s recent intake. If the total amount is approaching or has exceeded the pre-set cumulative dosage cap, the system generates an immediate alert. This flag prompts the healthcare professional to pause and review the treatment plan, possibly adjusting the dose, switching medications, or speaking with the patient.
This practice turns a simple prescription process into a dynamic safety check, fostering a collaborative effort between physicians and pharmacists to protect patient health. It’s a practical application of data to prevent harm in real time.
analyzing patient case studies
Analyzing patient case studies provides powerful, real-world lessons on the importance of cumulative dosage caps. These stories go beyond numbers and show the human impact of medication management. By examining specific instances where patients experienced harm, healthcare professionals can identify patterns and improve safety protocols for everyone.
A Common Scenario: The Risk of Multiple Doctors
Consider a hypothetical case: an elderly patient sees a primary care doctor for general health, a rheumatologist for arthritis pain, and a psychiatrist for anxiety. Each specialist, acting with the best intentions, prescribes medication. Without a centralized system to track the cumulative dose of all active ingredients, the patient is unknowingly taking a combination that puts a heavy strain on their liver over several months. Initially, their fatigue is dismissed as a symptom of old age.
A review of this case would show that an automated alert from a dosage cap system could have flagged the issue early. This would have prompted the specialists to coordinate, adjust the treatment plan, and prevent long-term organ damage. These case studies are not just for learning; they are the foundation for building smarter, safer healthcare practices.
computer modeling and risk evaluation
To evaluate overdose risks before they happen, experts now turn to sophisticated computer modeling. This technology uses predictive analytics to simulate how a medication might affect a person over time. Instead of waiting for problems to occur, these models forecast potential dangers based on a variety of factors.
These models are fed with large amounts of data, including a patient’s age, weight, kidney and liver function, and other medications they are taking. The computer then runs thousands of simulations to predict how the drug will accumulate in different types of patients. It’s like a digital crystal ball for pharmacology, showing potential outcomes without any real-world risk.
How Models Help Set Safe Caps
The main goal of this modeling is to identify the tipping point—the exact moment when a medication’s cumulative dose starts to become more harmful than helpful. By simulating long-term use, researchers can pinpoint a safe cumulative dosage cap. This data-driven approach allows for the creation of highly specific safety guidelines that are tailored to different patient populations, making medication management safer and more precise.
pharmacological perspectives of cumulative dosages
From a pharmacological perspective, cumulative dosage is all about how the body processes a drug over time, a field known as pharmacokinetics. This process includes absorption, distribution, metabolism, and excretion. The key factor in accumulation is the drug’s ‘half-life’—the time it takes for the body to eliminate half of the dose.
Drugs with a long half-life are cleared from the body slowly. If doses are taken more frequently than the half-life period, the drug doesn’t have enough time to be fully eliminated before the next dose arrives. As a result, the concentration of the drug in the bloodstream gradually builds up, or accumulates, potentially reaching toxic levels even when the individual doses are considered safe.
The Role of Liver and Kidneys
The liver and kidneys are the body’s primary filtration and processing centers for medications. The liver metabolizes (breaks down) drugs, while the kidneys excrete them through urine. When the cumulative dose of a medication becomes too high, it can overwhelm these organs. This overload can impair their function, which in turn slows down drug elimination even more, creating a dangerous cycle of increasing drug concentration and organ strain. Cumulative dosage caps are therefore set with a deep understanding of these biological processes to protect vital organ functions.
regulatory guidelines and safety standards
Cumulative dosage caps are not established arbitrarily; they are guided by strict regulatory guidelines and safety standards set by government agencies like the Food and Drug Administration (FDA). These organizations are responsible for protecting public health by ensuring that medications are both effective and safe for long-term use. Their guidelines are based on extensive scientific evidence and data analysis.
These standards are often part of a drug’s official labeling and can be legally binding for both manufacturers and healthcare providers. The goal is to create a unified, national approach to medication safety, preventing individual clinics or doctors from making isolated judgments that could lead to patient harm.
From Clinical Trials to Mandated Protocols
The process begins during a drug’s development. Data from clinical trials is carefully analyzed to identify the point at which a medication’s cumulative exposure starts to pose a risk. Based on this evidence, regulatory bodies establish mandated safety protocols. These can include required warnings, specific monitoring instructions, and firm dosage limits that must be followed to ensure patient safety is the top priority in all medical practices.
real-world instances of overdose events

Real-world overdose events often don’t match the dramatic scenes shown in movies. Instead, they are frequently quiet, gradual, and completely unintentional. These incidents highlight the critical need for awareness about the cumulative effects of common medications, not just powerful prescriptions.
The Common Case of Acetaminophen
A classic real-world example involves acetaminophen, an active ingredient in many over-the-counter pain relievers and cold remedies. A person might take the maximum recommended dose of a pain reliever for a headache. At the same time, they could be taking a multi-symptom cold medicine to treat a cough and runny nose, not realizing it also contains a full dose of acetaminophen.
Over several days, this innocent mistake leads to a cumulative overdose. The total amount of the drug builds up in their system, leading to severe and sometimes irreversible liver damage. These are not rare occurrences; they are preventable tragedies that underscore why tracking total intake is so vital for public safety.
data trends and statistical analysis
By analyzing large sets of health data, we can uncover hidden trends in medication use and overdose risks. This field, often called population health management, uses statistical analysis to look at anonymized data from thousands or even millions of people. It’s like having a bird’s-eye view of how medications are being used across entire communities.
This analysis can reveal which drugs, or combinations of drugs, are most frequently associated with cumulative overdose events. It also helps identify specific groups of people who might be at higher risk, such as older adults or individuals with certain health conditions. These insights are not just academic; they are vital for public health.
Turning Data into Actionable Safety Measures
The trends discovered through this statistical work directly influence how cumulative dosage caps are developed and refined. For instance, if data shows a spike in liver-related issues among patients taking a specific medication for more than six months, health authorities can use that information to recommend a new, lower cumulative cap. It’s a proactive approach that uses real-world evidence to make prescribing safer for everyone.
healthcare policies on dosage limits
Beyond individual clinical decisions, many healthcare systems implement overarching policies on dosage limits to ensure patient safety on a large scale. These are not just recommendations; they are formal rules put in place by hospitals, insurance companies, and public health programs. The goal is to create a standardized safety net that protects all patients within that system.
These policies often work through administrative and financial controls. For example, a health insurance policy might automatically deny payment for a prescription refill if it puts a patient over the established cumulative dosage cap for a specific drug. This creates a ‘hard stop’ in the system, forcing a review of the prescription.
How Policies Are Enforced
Enforcement usually happens at the pharmacy level. When a pharmacist processes a prescription, their system communicates with the insurance provider. If a policy flags the dose as too high, the transaction is blocked, and the pharmacist is prompted to contact the prescribing doctor. This system-wide approach helps catch potential errors that might otherwise be missed, especially when a patient sees multiple doctors who are unaware of each other’s prescriptions. It’s a powerful way to enforce safety standards uniformly.
patient education for overdose prevention
The most important part of preventing an overdose is the person taking the medication. Patient education empowers you to take an active role in your own safety. This means understanding what you are taking and why. It’s about turning passive pill-taking into active health management.
A critical first step is to read every label, including on over-the-counter products. Look for the ‘Active Ingredients’ section. You might be surprised to find that your allergy pill and sleep aid contain similar ingredients, which can add up to a dangerous cumulative dose.
Take Charge of Your Medication Safety
Never hesitate to ask your doctor or pharmacist questions. A simple question like, ‘Will this new prescription interact with my other medications?’ can be life-saving. It is also vital to maintain a complete and updated medication list—including vitamins, supplements, and herbal remedies—and share it with all of your healthcare providers. You are the final, and most crucial, checkpoint in your own treatment plan.
technology aiding dosage tracking
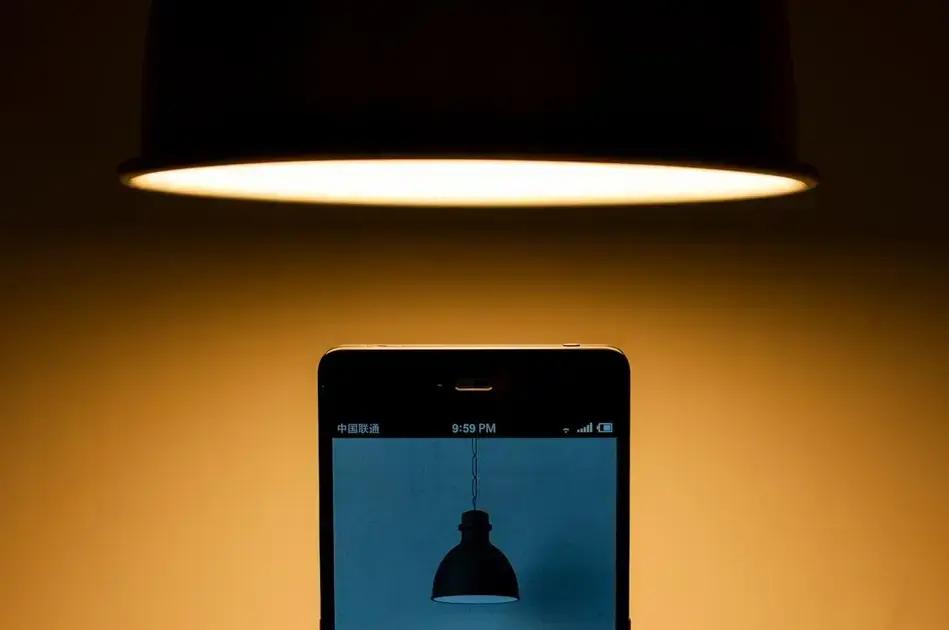
Technology has transformed how we track our health, and medication management is no exception. Gone are the days of relying solely on memory or handwritten logs. Today, a range of digital tools can help you accurately track your dosage, making it easier to stay within safe cumulative limits.
These technologies provide real-time feedback and can automatically calculate your total intake over a given period. This removes the guesswork and provides a clear picture of your medication use, empowering you to avoid accidental overdose.
Smart Tools for Safer Medication Use
Some of the most helpful tools include smartphone apps that allow you to set reminders, scan barcodes on medicine bottles to log doses, and track cumulative amounts. Many can also alert you if you are approaching a pre-set limit. Smart pill bottles go a step further; they can glow when it’s time to take a dose and send a notification to your phone if you forget. More advanced technologies like wearable sensors are also emerging, which may one day monitor drug levels in the body directly. This data can often be shared with your doctor, creating a more complete and accurate health record.
comparison between traditional and modern practices
Traditionally, medication management relied heavily on patient memory and handwritten notes. Doctors and pharmacists depended on patients to report what they were taking, a system prone to error and incomplete information. This approach was largely reactive; problems like cumulative overdose were often discovered only after a patient began showing symptoms of toxicity. Communication between different specialists could be slow, leaving dangerous gaps in a patient’s medication history.
From Reactive to Proactive Safety
Today, modern practices have shifted towards proactive safety. Integrated systems like Electronic Health Records (EHRs) and pharmacy databases automatically track a patient’s prescriptions from all sources in real-time. Paired with patient-facing tools like smartphone apps and smart pill bottles, this technology creates a comprehensive safety net. Instead of waiting for a problem to happen, these modern digital tools can flag a potential cumulative overdose risk before the last pill is even dispensed, allowing for immediate intervention.
challenges in implementing cumulative caps
While cumulative dosage caps are a powerful safety tool, implementing them effectively comes with significant challenges. One of the biggest hurdles is fragmented health data. A patient’s medical information is often scattered across different doctors’ offices, hospitals, and pharmacies, none of which may communicate with each other. This makes it nearly impossible to get a complete and accurate picture of all the medications a person is taking.
The Challenge of Untracked Medications
Another major blind spot is the use of over-the-counter (OTC) products. A patient might be taking prescribed medication while also using OTC pain relievers or cold remedies. Since these purchases are not tracked in official health records, they don’t get factored into the cumulative dose calculation, creating a hidden risk.
Furthermore, in a clinical setting, healthcare professionals can suffer from ‘alert fatigue.’ If systems generate too many warnings, staff may become desensitized and start to ignore them, potentially missing a critical alert about a genuine overdose risk. Finding the right balance for these alerts is a constant challenge.
future advancements in overdose monitoring
The future of overdose monitoring is shifting towards truly personalized and real-time solutions. Instead of broad safety guidelines, advancements aim to tailor dosage limits specifically to you. This will bring a new level of precision and safety to medication management.
AI-Powered Personalization and Wearables
Imagine systems using artificial intelligence (AI) to analyze your unique genetic profile, lifestyle habits, and health data to predict exactly how you’ll respond to a medication. This goes a step beyond current computer models. Paired with this, wearable sensors, like a discreet skin patch or an advanced smartwatch, could continuously measure the actual drug levels in your body. If these levels start to approach a personalized danger zone, both you and your doctor could receive an immediate alert.
This seamless integration means future health monitoring will be dynamic and constantly updated. It promises a proactive system where potential overdoses are flagged based on your body’s real-time response, creating the ultimate safety net.
strategies for balancing effectiveness and safety
The ultimate goal of any medication plan is to find the perfect balance between effectiveness and safety. The dose must be strong enough to provide the intended therapeutic benefit, but not so high that it poses a risk of harm or overdose. This ideal range is often called the therapeutic window, and staying within it is a dynamic process.
Finding the Sweet Spot
A key strategy for achieving this balance is the principle of ‘start low and go slow.’ Doctors often begin treatment with a lower dose and gradually increase it over time, carefully monitoring the patient’s response. This allows them to find the lowest possible dose that is still effective for that individual, which naturally minimizes risk.
This is a collaborative effort between the patient and the provider. Regular follow-ups and open communication are essential. By reporting how you feel and any side effects you experience, you provide the crucial information your doctor needs to fine-tune your treatment, ensuring the scale is always tipped in favor of health and safety.
Take Control of Your Medication Safety with Cumulative Dosage Caps
Setting cumulative dosage caps is a smart and simple way to prevent accidental overdoses. As we’ve seen, the total amount of a medication you take over time matters just as much as a single dose. This modern approach shifts medication management from being reactive to proactive, putting your safety first.
From electronic health records that alert your doctor to smartphone apps that help you track your intake, technology provides a powerful safety net. However, the most important part of this team is you. By understanding your medications, reading labels, asking questions, and keeping all your providers informed, you play the final and most critical role in your own health journey.
Ultimately, managing your treatment is about finding that perfect balance between effectiveness and safety. Cumulative dosage caps are a key strategy in this effort. Stay informed, stay engaged, and use these tools to ensure your medications help you without causing unintended harm.
FAQ – Understanding Cumulative Dosage Caps for Medication Safety
What exactly is a cumulative dosage cap?
It’s a pre-set safety limit on the total amount of a specific medication you take over a set period (like a week or month). It’s designed to prevent the drug from gradually building up to a harmful level in your body.
Can I accidentally overdose on over-the-counter (OTC) medicines?
Yes. A common risk is taking multiple different products, like a pain reliever and a cold medicine, that both contain the same active ingredient. The total amount can add up to a dangerous cumulative dose without you realizing it.
Why is it important to tell my doctor about all medications, including supplements?
Your doctor needs a complete picture to ensure your safety. Unlisted medications, vitamins, or supplements can interact with your prescriptions or contribute to cumulative effects. Sharing everything helps prevent accidental overdoses.
How does technology help manage dosage safety?
Modern tools like electronic health records can automatically alert doctors and pharmacists if a prescription exceeds a cumulative cap. At home, smartphone apps and smart pill bottles can help you track your intake and avoid mistakes.
What is the ‘therapeutic window’ of a medication?
The therapeutic window is the ideal concentration range for a drug in your body. Below this range, it may not work effectively, and above it, it can become toxic. Careful dosage monitoring helps keep you safely within this window.
Why did my doctor start me on a very low dose of a new medication?
This is a common safety strategy known as ‘start low and go slow.’ It allows your doctor to find the lowest dose that is still effective for you, which helps achieve the best balance between the medication’s benefits and its risks.



